
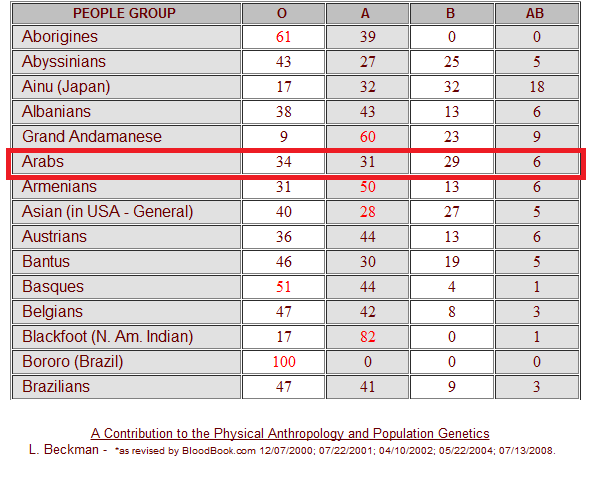
How RHD Genotyping Improves Clinical Management of Obstetrics Patients & Transfusion Recipients Many, but not all, could be treated as RhD-positive however, depending on the RHD genotype. In standard serologic tests, these individuals will type as RhD-negative, and thus are usually treated as such. Individuals with partial D types are at risk for clinically significant sensitization and should be treated as RhD negative for transfusion and candidates for Rh immune globulin if the fetus is RhD positive.ĭEL types have been most commonly observed in patients of Asian ethnicity. Partial D types are more common among patients of African ancestry, but are also found in Caucasian populations. Risk for individuals with weak D types other than 1, 2 or 3 is unknown, but no clinically significant events have been reported to date. Individuals with Weak D Types 1, 2 or 3 are not at risk of RhD sensitization or hemolytic disease (HDFN) when the fetus is RhD-positive. Between 1 – 3% of Caucasians have a weak D type, and the vast majority (~95%) of these individuals have Weak D Types 1, 2 or 3, as determined by RHD genotyping. Weak D types are more common in Caucasians with European ancestry. Which RhD Variants Are Observed Across Different Ethnic Groups? The goal is to avoid pregnancy complications and transfusion complications particularly for females of child bearing potential. For individuals, including pregnant women, with either a weak D type or variable or discordant RhD typing, a College of American Pathologists (CAP) and AABB Work Group recommends that RHD genotyping be performed to correctly determine whether the individual should be treated as RhD-positive or RhD-negative for Rh immune globulin (RhIG) prophylaxis and for blood transfusion.
#A NEGATIVE BLOOD TYPE ETHNICITY CODE#
Well over 300 RHD gene variants that code for weak D, partial D and DEL/inactive D types have been reported to date. While it is common for RhD status to be first evaluated by typing of the red blood cells, the most accurate method to determine RhD status and risk of sensitization (alloimmunization) is by RHD genotyping. What Is the Best Way to Evaluate RhD Variation? Individuals with DEL types will most likely be classified serologically as RhD-negative. DEL types, on the other hand, are characterized by extremely low levels of RhD antigens that can’t be detected by routine testing. These individuals can become sensitized to RhD positive red cells during pregnancy or following transfusion.

Partial D types are characterized by amino acid substitutions in the RhD proteins leading to the expression of an RhD antigen lacking epitope(s). Two other categories of RhD variation, partial D types and DEL types, are infrequent in Caucasians, but are found in 6% of African Americans and 1% of Asians, respectively. Of the remaining 15% that type as RhD-negative, a small percentage of individuals (~3 percent of those typed as RhD-negative) have weak D types, RhD variants characterized by red blood cells that are initially nonreactive or weakly reactive but agglutinate moderately or strongly with the addition of anti-human globulin. In the U.S overall, approximately 85 percent of pregnant women type (phenotypically) as RhD-positive. Unlike other blood group antigens that routine laboratory testing detects as either positive or negative, RhD antigen testing may be unclear or ambiguous due to genetic variation associated with inheritance and ethnicity. RhD antigen status is also important for blood transfusion recipients, as RhD-negative individuals who receive RhD-positive blood may also become sensitized (alloimmunized). Evaluation of RhD antigen status is particularly important for pregnant women, as exposure of RhD-negative women to a RhD-positive fetus may cause hemolytic disease of the fetus or newborn (HDFN), in which the mother becomes sensitized (makes an immune antibody) and the maternal antibody crosses the placenta and attaches to the red blood cells of the fetus (erythroblastosis fetalis).


 0 kommentar(er)
0 kommentar(er)
